In their handling of the recent vaping scare, U.S. health authorities have unintentionally served the public poorly.
By George Gay

If there was one thing, and one thing only, that participants took away from September’s Global Tobacco & Nicotine Forum (GTNF), it was surely the idea that vaping precepts in the U.S., which have never appeared to form a coherent whole, were starting to resemble a witch’s brew. But how can this be? After all, vaping policy in the U.S. is guided by the Food and Drug Administration (FDA), which, in turn, makes decisions on the basis of science not on the basis of witchcraft or alchemy.
There are clearly a lot of issues playing out here, but, according to Konstantinos Farsalinos, a research fellow at the Onassis Cardiac Surgery Center in Athens, Greece, one problem is that science is playing only a “very small” role in the vaping debate in the U.S., and even then, it is sometimes being misused to support “emotional aspects” of the debate. “You are seeing such a distortion of scientific facts that it is extremely disappointing for all of us outside the U.S.,” he told me during a telephone interview in November.
But I should point out that Farsalinos, who gave a presentation at the GTNF held Sept. 24–26 in Washington, D.C., does not subscribe to conspiracy theories about scientists deliberately misleading the public. I asked him about the reaction by the Centers for Disease Control and Prevention (CDC) to an outbreak of acute lung disease among people using vapor devices—an outbreak that had become widely publicized only shortly before the GTNF was held. At that time, the CDC had apparently concluded that the outbreak, which by then had occurred only in the U.S. and, in respect of a single case, in Canada, could be due to vaping with nicotine alone. The first item on its list of advice concerning the illness was that people should “consider refraining from using e-cigarette, or vaping, products, particularly those containing THC [tetrahydrocannabinol].” This seemed to be an odd conclusion to draw given that, as Farsalinos pointed out in his presentation, people had been vaping with nicotine for more than 10 years around the world while the inhalation of THC by evaporating THC oils was a much more recent phenomenon.
Nevertheless, other presentations made at the GTNF indicated that the CDC’s approach had spooked vapers, with some representatives of vape shop chains indicating that sales had dropped by up to 20 percent following the agency’s initial announcements and that the footfall of smokers looking to try vaping had fallen by about 50 percent.
The easiest and most reasonable explanation for the way the CDC scientists behaved was their predisposition to taking a negative view of vapor products, Farsalinos said, before adding that he wasn’t suggesting the CDC scientists had set out intentionally to misinform the public or to cause harm. Speaking to me on Nov. 9, Farsalinos said the CDC had reported the previous day that all of the 29 cases of acute lung disease it had subjected to bronchoalveolar lavage analyses had revealed the presence of vitamin E acetate, which was a marker of THC oil usage. The CDC now almost accepted that all the cases it had examined had occurred among those who were using THC, he added, but, because of its earlier stance, nearly everyone was misinformed. Opinion polls showed that more people in the U.S. believed that nicotine vaping was dangerous than that THC oil inhalation was dangerous.
So the CDC’s approach, Farsalinos said, and all the campaigns that were mounted had resulted in a “gross misinformation of the public,” something that was not unexpected when you examined what kinds of arguments the CDC scientists had been using, what kinds of press statements they had been issuing and what kinds of official reports they had been releasing. “I’m not saying this was intentional, but the scientists at the CDC—those at the FDA made a better case much sooner—allowed themselves to be influenced largely by the negative attitude toward electronic cigarettes in general, and they have unintentionally served the American public badly,” he said.
Confirmation bias
This of course raises a question. The people at the CDC are scientists, so why would they give way to emotion and prejudice: Why didn’t they stick to the science? Farsalinos said he believed this was a typical case of confirmation bias. The scientists had very strong negative opinions about electronic cigarettes, and this influenced the way they looked at the data. “One of the arguments they were using was that not all of the lung disease sufferers reported THC use,” he said. “But this is a naive argument because it is well known that people misreport. Some people will avoid reporting the use of THC, especially if they have been using illicit THC in states where it is illegal to use THC.”
Farsalinos suggested also that the CDC scientists had lost track of an important aspect of such outbreaks. Epidemiology had demonstrated that while it might be possible theoretically for one epidemic to be generated by two very different causes, this almost never happened in practice, he said. So, it was not possible that both THC oils and nicotine liquids, which were two extremely different products, could have caused the same epidemic.
And it would seem that the CDC required higher levels of proof of causal links in the case of the recent lung disease outbreak than it had in relation to other health problems. The causes of recent and fairly recent outbreaks of salmonella poisoning and Legionnaires’ disease, for example, had been rightly identified and accepted on the basis that about 80 percent to 85 percent of sufferers reported being in contact with the suspected cause. In the case of the recent lung disease outbreak, however, the CDC scientists needed higher levels of proof of causal links, and this again seemed to be a case of confirmation bias.
Accepting the obvious
While the FDA came out of the lung disease furor in better shape than the CDC, it too has had its problems, and I asked Farsalinos how it had reached the point where the FDA’s science seemed not to be getting harm reduction policy to the place where it should be. At this point, he turned to the issue of snus. Snus, he said, was a product whose harm reduction credentials were supported by a level of evidence that you could not even dream of in the case of any other tobacco or nicotine product. “We’re not talking about chemistry, toxicology, cell studies or animal studies,” he said. “We are talking about hardcore evidence: clinical evidence, long-term studies. We have meta-analyses of epidemiological and clinical data. We have known about this for 10 years at least.”
Nevertheless, it took the FDA many years to accept the obvious—that snus use is a less harmful alternative to smoking, he said. (On Oct. 22, the FDA announced that it had authorized the marketing of eight Swedish Match USA snus products as modified-risk tobacco products.) And this was down to the rigidity of such organizations when it came to anything that was related to tobacco. It showed a dogmatic approach that said smokers should have no option but simply to quit their habit. “It would have been ideal if people were able to simply quit without using any aid or alternative products,” Farsalinos added. “The problem is [that] not all smokers are able to quit. We cannot provide them with very effective smoking cessation medications.
“Instead of seeing harm reduction products as placing an obligation on the scientific community to provide as many tools as possible, additional tools to help people quit, parts of the scientific and public health community are doing the opposite. They are depriving smokers of an additional option [electronic cigarettes] to quit, which is absurd … it is literally absurd.”
Farsalinos said there was, of course, a need for well-implemented restrictions and regulations in respect of vapor products, but the U.S. had done very little in this direction. It basically had no regulation, and it did not enforce the rules it did have, such as the ban on sales to young people. It had failed in enforcing this ban and was punishing smokers because of that failure. And worse, it was causing people who had used vapor products to quit smoking in the past to relapse by encouraging them to believe that they were going to be more harmed by vaping than by smoking.
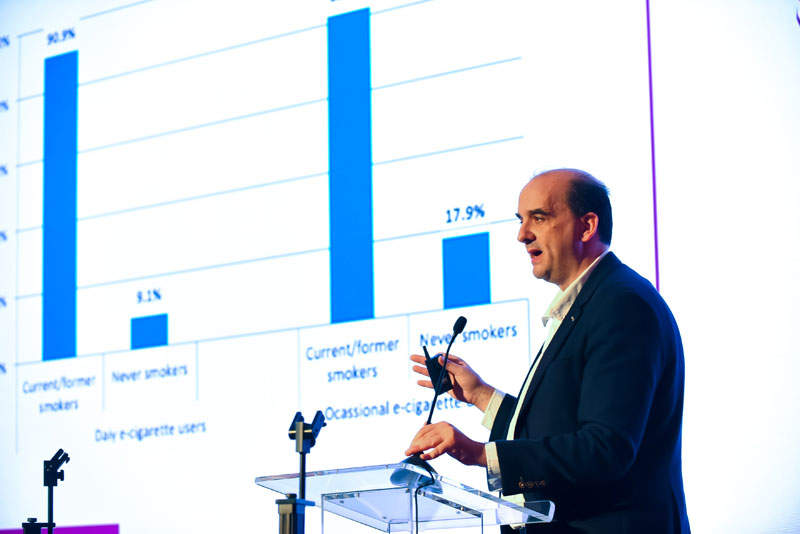
Farsalinos was also critical about the misuse of evidence in respect of vaping among young people. “We should definitely monitor it, and we should definitely try our best to prevent use by never smokers and by youth, but this is becoming an emotional obsession which has very little to do with the evidence.” The evidence pointed to the fact that vaping among young people was largely experimental and infrequent, he added, and it was largely confined to adolescents with a smoking history.
Finally, Farsalinos said it was ironic that while, around the world, the concept of harm reduction was generally accepted, it faced more resistance in the case of tobacco. “I would accept a rejection of a harm reduction principle if we had the tools to make all or the vast majority of smokers quit,” he said. “But we don’t. When you have the most successful smoking cessation medication having a success rate of 25 percent in the long term, what is going to happen with the rest of the smokers? When you have smoking cessation medications that are unpopular among smokers, what are you going to do with the rest—punish them because they don’t want to use the medication or because they failed to quit with medication? It doesn’t make sense.”