The coronavirus crisis has reinforced anti-tobacco activists’ existing worldviews.
By Stefanie Rossel
The coronavirus pandemic could have been a chance for public health authorities and governments to promote tobacco harm reduction (THR). Instead, they resorted to well-known, tried-yet-unproven remedies, restricting sales channels or banning tobacco products altogether.
To warn against smoking, an activity linked to respiratory problems, appears to be a no-brainer when a deadly virus with the potential to cause acute lung failure is spreading rapidly around the globe. Yet many governments and public health authorities went much further. The Covid-19 outbreak amplified tobacco control policies that had been in circulation for decades, creating an opportunity to implement measures that would otherwise be unthinkable.
Based on the assumption, not scientific evidence, that people who smoke or vape may be at greater risk for Covid-19, anti-tobacco campaigners considered the pandemic the perfect opportunity to suggest that smokers and vapers quit both habits, preferably through willpower but otherwise with the aid of nicotine-replacement therapy (NRT).
In times of pressure, well-researched subjects, such as nicotine addiction, the differentiation between tobacco and nicotine and the method of nicotine delivery, appear to play an even smaller role than usual. How else to explain the decision of many jurisdictions to close vape shops during the first weeks of the pandemic? Even the U.K., a bastion of enlightenment in terms of tobacco harm reduction, ranked vape shops as “nonessential businesses.” As recently as 2019, Public Health England had reaffirmed its recommendation of vaping, which it considers to be 95 percent less harmful than smoking, as a cessation tool.
Critics warned the closure of U.K. vape shops would drive vapers back to cigarettes—a worry borne from a study carried out in May by The Guardian. The survey found that about 2.2 million people are smoking more than usual while 4.8 million are smoking the same amount and 1.9 million have decreased the amount they smoke. The rise in smoking has been attributed to heightened stress and anxiety related to the lockdowns. Smoking is also used as an excuse to go outside. The freedoms that come with working from home, without the restrictions that apply in the workplace, have also aided in the rise, the study’s authors said.
South Africa went furthest by banning tobacco and vapor product sales altogether. Imposed to slow the spread of the coronavirus, the prohibition had serious unintended consequences. The country’s illicit cigarette trade, which, according to Bloomberg, already cost the government ZAR7 billion ($401 million) a year in lost tax revenue before the prohibition, exploded following the ban.
A survey of 16,000 people conducted by the University of Cape Town found that 90 percent of smokers who wanted to buy cigarettes during the lockdown were able to do so, albeit at inflated prices. Not only did the ban turn thousands of consumers into lawbreakers, it also forced people to travel and interact with dealers who had potentially touched numerous other people while selling their wares. At the time of writing, the tobacco ban remained in place even as the government had started easing other restrictions, such as that on selling alcohol.
Critics warned the closure of U.K. vape shops would drive vapers back to cigarettes—a worry borne from a study carried out in May by The Guardian. The survey found that about 2.2 million people are smoking more than usual while 4.8 million are smoking the same amount and 1.9 million have decreased the amount they smoke. The rise in smoking has been attributed to heightened stress and anxiety related to the lockdowns. Smoking is also used as an excuse to go outside. The freedoms that come with working from home, without the restrictions that apply in the workplace, have also aided in the rise, the study’s authors said.
South Africa went furthest by banning tobacco and vapor product sales altogether. Imposed to slow the spread of the coronavirus, the prohibition had serious unintended consequences. The country’s illicit cigarette trade, which, according to Bloomberg, already cost the government ZAR7 billion ($401 million) a year in lost tax revenue before the prohibition, exploded following the ban.
A survey of 16,000 people conducted by the University of Cape Town found that 90 percent of smokers who wanted to buy cigarettes during the lockdown were able to do so, albeit at inflated prices. Not only did the ban turn thousands of consumers into lawbreakers, it also forced people to travel and interact with dealers who had potentially touched numerous other people while selling their wares. At the time of writing, the tobacco ban remained in place even as the government had started easing other restrictions, such as that on selling alcohol.

(Photo: Kentucky Bioprocessing)
Spreading misinformation
The South African government based its tobacco ban on advice from the World Health Organization (WHO), which maintains that although research is still being carried out, there is reason to believe that smokers would be more adversely affected than nonsmokers if they contracted Covid-19. Similar claims were made by authorities in other jurisdictions. Vaping, for example, was singled out as a risk factor for Covid-19 by New York City’s mayor, Bill de Blasio, the U.S. surgeon general and the U.S. National Institute on Drug Abuse. Even the U.S. Food and Drug Administration lumped vaping with smoking in the coronavirus context—but backtracked quickly in the absence of proof.
“Such misinformation ultimately harms the credibility of such bodies,” says David Sweanor, chair of the Advisory Board for the Center for Health Law, Policy and Ethics at the University of Ottawa. “Due to the role of the internet in compiling information and social media for sharing it, deception is no longer a viable strategy. It was never an ethical one. These bodies have been engaging in credibility self-immolation at a time when credibility and trust in government health bodies is essential to their role in countering Covid-19.”
While there are plenty of studies on the subject now, research into the relationship between tobacco use and Covid-19 remains inconclusive. Early in the pandemic, however, two meta-analyses found that smoking was not a risk factor for Covid-19 hospitalization. On the contrary, one of the researchers, Konstantinos Farsalinos, a cardiologist at the university of Patras, Greece, suggested that nicotine might even reduce the risk of contracting the coronavirus.
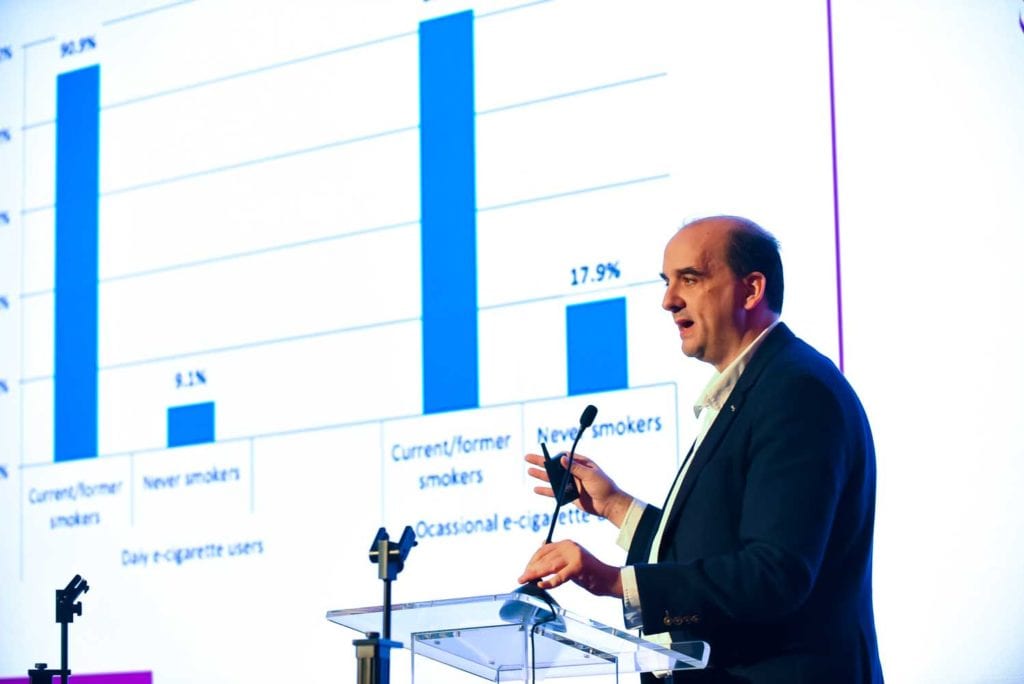
When examining Chinese data on Covid-19 patients, Farsalinos observed an unusually low prevalence of current smoking among Covid-19 patients compared to the expected prevalence based on smoking rates in China. While about one third of Chinese adults smoke, only 9.6 percent of hospitalized Covid-19 patients were smokers. Studies in the U.S., France and Germany noticed similar discrepancies between the share of smokers among hospitalized Covid-19 patients and their share in the general population.
The protective effect, Farsalinos speculated, could be linked to the downregulation of angiotensin-converting enzyme 2 (ACE2) expression. The coronavirus is known to use the ACE2 for cell entry. In a peer-reviewed paper published in Toxicology Reports, Farsalinos also suggested that by maintaining or restoring the cholinergic anti-inflammatory system, nicotine could control the release of pro-inflammatory cytokines and thus prevent or suppress a “cytokine storm.” Cytokines are proteins that help organize the body’s immune response to infections. A cytokine storm, often found in patients with a severe form of Covid-19, represents a failure of the inflammatory response to return to normal operation, which can potentially lead to catastrophic tissue damage.
Jean-Pierre Changeux, professor emeritus of molecular neurobiology at College de France and Institut Pasteur, went a step further. To test the protective properties of nicotine, he initiated a human trial in May. It involved groups of healthcare workers and patients wearing nicotine patches and other groups wearing placebo patches. According to Reuters, similar testing will be carried out on 400 hospitalized Covid-19 patients to understand if nicotine alters the progress of the disease. While the scientists emphasized that their research wasn’t meant to encourage smoking, French authorities limited sales of NRTs to avoid a shortage.
Harmful approach
The idea that nicotine may have benign properties, that the much-demonized tobacco plant might contribute something positive, fits poorly with anti-tobacco campaigners’ worldviews. When British American Tobacco announced in April that its subsidiary Kentucky BioProcessing had made a breakthrough in developing a tobacco plant-based vaccine candidate for Covid-19 (see “Shots on Goal,” Tobacco Reporter, June 2020), the WHO was quick to warn governments against engaging with the tobacco industry. Partnership with the tobacco industry, the global health body stated, undermines governments’ credibility in protecting population health as there is “a fundamental and irreconcilable conflict between the tobacco industry’s interests and public health policy interests.”
The WHO’s May 11 statement on tobacco use and Covid-19 may be read in a similar way—as a preemptive discreditation of all studies that might not be in line with the organization’s ideology. “WHO stresses the importance of ethically approved, high-quality, systematic research that will contribute to advancing individual and public health, emphasizing that promotion of unproven interventions could have a negative effect on health.”
The organization has been criticized for its handling of the coronavirus crisis. It has been accused of acting too slow to halt the pandemic and of opaqueness under influence from China. “The WHO is not helping public health,” said Tim Andrews, founder and president of the Australian Taxpayers’ Alliance, in a webinar held by the Reason Foundation. “Just think of its failures in the Covid-19 crisis.”
The WHO has a track record of preventing reduced-risk products (RRPs), an approach that has killed millions of people, according to Andrews. The WHO, he says, has strayed from its original aims, a development that became visible when it initiated the Framework Convention on Tobacco Control in 2003. “As the policies of the WHO failed, people at the same time adopted RRPs, thus smoking rates declined,” said Andrews. “The WHO had two choices: either accept e-cigarettes or double down on their measures. They opted for the latter.”
The more e-cigarettes and heated-tobacco products prove to be effective harm reduction tools, the more the WHO regulates against them, according to Andrews. “If people are scared of RRPs, they will stick to combustible cigarettes,” he cautioned. “The WHO has been deliberately lying and spreading misinformation.”
How the misunderstanding of nicotine will impact THR in the long run remains to be seen. Sweanor remains confident. “I am optimistic that Covid-19 will lead to a reexamination of public health bodies and public health policies in general,” he says. Many of the failings with nicotine, such as acting on unscientific authoritarian impulses rather than focusing on pragmatically reducing risks for the most vulnerable, have been tragically repeated with Covid-19, according to Sweanor. “If basic public health principles and ethics could be reestablished in major health bodies such as the WHO and CDC [the U.S. Centers for Disease Control and Prevention], it could lead to breakthroughs not just on pandemic responses and nicotine but on a wide range of other pressing issues.”