A patent dispute derails the U.S. rollout of IQOS.
TR Staff Report
The deadline of Tobacco Reporter’s December print edition coincided with one for the U.S. Trade Representative to overturn a ruling preventing Altria Group subsidiary Philip Morris USA from importing Philip Morris International’s IQOS tobacco-heating device following a patent dispute.
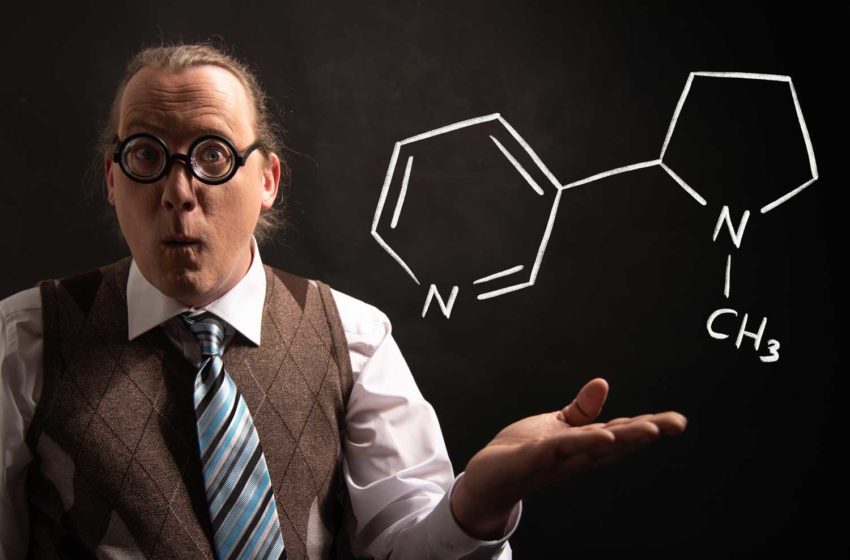
On Sept. 30, the International Trade Commission upheld an initial determination that PMI’s IQOS device infringes patents owned by BAT. As a result of the ITC ruling, Philip Morris USA has been barred from importing PMI’s IQOS 2.4, IQOS 3 and IQOS 3 Duo heat-not-burn traditional cigarette products. It was also ordered to halt future sales of those products—marketed as Marlboro HeatSticks—already in the U.S.
Altria Group asked trade representative Katherine Tai to overturn the ban. Tai had 60 days to do so. By Nov. 30, however, the U.S. Trade Representative’s office confirmed to Bloomberg that no action had been taken by Tai, meaning the IQOS import ban stands.
BAT welcomed the development. “Today’s announcement provides a measure of success for our enforcement of intellectual property rights to ensure we can continue to innovate, as is common practice among innovation-based industries,” Gareth Cooper, BAT’s assistant general counsel, said in a statement. “As we have strenuously noted, there was no reason to overturn the policy.”
Altria expressed disappointment with the decision. “We continue to believe that the plaintiff’s patents are invalid and that IQOS does not infringe on those patents,” the company said in a statement.
“The ITC’s importation ban makes the product unavailable for all consumers who have switched to IQOS, reduces the options for the over 20 million smokers looking for alternatives to cigarettes and ultimately is detrimental to the public health.”
This sentiment was echoed by Gregory Conley, president of the American Vaping Association, at the time of the ITC’s Sept. 30 decision.
“By potentially denying them the opportunity to switch to a harm reduction production IQOS, the real losers of this protracted court battle could end up being American adult smokers,” Conley said.
“While some may use vaping, snus or pouches in the absence of IQOS, far too many American adults will choose to just smoke cigarettes instead.”
The U.S. Food and Drug Administration authorized IQOS for sale in April 2019. The products debuted in test markets in Atlanta in October 2019 and Richmond, Virginia, in November 2019. During the second quarter, Philip Morris USA expanded retail distribution of Marlboro HeatSticks into the Triad and other metro areas of North Carolina as well as northern Virginia and Georgia.
In immediate financial terms, the import ban has limited impact on PMI and Altria. IQOS in the U.S. is currently not a meaningful contributor to the companies’ earnings, according to Morgan Stanley. Nonetheless, IQOS is a key element in Altria’s shift away from traditional tobacco products, which have seen falling demand. To achieve its mission “to responsibly lead the transition of smokers to a smoke-free future,” Altria will need a viable alternative to combustible cigarettes in its portfolio.
Altria will likely appeal to the U.S. Court of Appeals for the Federal Circuit, which handles patent lawsuits. That process could take up to a year to reach a decision, with the likelihood of a successful appeal not favorable, according to industry analysts.
In the worst-case scenario for Altria and Philip Morris, the two companies would have to go back to the drawing board, moving production to the U.S. or changing up the design enough to avoid patent infringement claims.














 India closely adheres to the WHO’s abolitionist stance, as evidenced by the country’s 2019 ban on vape products. “My understanding is there is a general denial of harm reduction approaches among governmental stakeholders,” Chowdhery says. “I am not sure, though, how the bans are evaluated or if there is a mechanism for that, though I do keep hearing about smuggling of these goods going up through everyday reports of seizures.
India closely adheres to the WHO’s abolitionist stance, as evidenced by the country’s 2019 ban on vape products. “My understanding is there is a general denial of harm reduction approaches among governmental stakeholders,” Chowdhery says. “I am not sure, though, how the bans are evaluated or if there is a mechanism for that, though I do keep hearing about smuggling of these goods going up through everyday reports of seizures.