How prioritizing evidence-based harm reduction strategies for smoking can improve healthcare
By Kgosi Letlape
Evidence-based harm reduction strategies, known for mitigating the adverse effects of persistent unhealthy behaviors and substances, focus on reducing health risks while acknowledging the difficulty of achieving complete abstinence.
Since the mid-1900s to late 1900s, efforts such as syringe exchange programs, safer injection facilities, overdose prevention programs and policies, and opioid substitution treatment have been implemented to reduce the adverse health, social and economic consequences of illicit drug use. These approaches have been proven to reduce transmission of HIV and other infections, increase users’ access to other medical and social services, and increase enrollment in detoxification treatment, without increasing social disorder in the community. Other examples include health education and provision of free condoms to help reduce HIV and other sexually transmitted infections and unwanted pregnancy, especially among the youth.
Likewise, these behaviors that are difficult to cut down on or eradicate should equally be extended and applied to tobacco. A formal tobacco harm reduction strategy is urgently needed for smokers, which would provide them with safer noncombustible alternatives to traditional cigarettes.
More than 1.1 billion people across the world smoke tobacco, consuming nearly 5 trillion cigarettes a year. Around 37 billion of those are smoked by South Africans. South Africa has an extremely high number of smokers; approximately two out of every five men and one in 10 women over the age of 15 smoke.
The impact on personal health and the healthcare system, and the economic implications are massive. Smokers are three times to five times more likely than nonsmokers to die prematurely, such that more than 25,000 South Africans over the age of 35 die each year from smoking-related diseases. That means one in 10 deaths are related to smoking. In our hospitals, nearly 139,000 admissions and just under 3 million outpatient visits every year are attributable to smoking. Add to that the more than 621,000 workdays lost due to illness from smoking, and the annual cost to the economy works out to about ZAR42 billion ($2.3 billion).
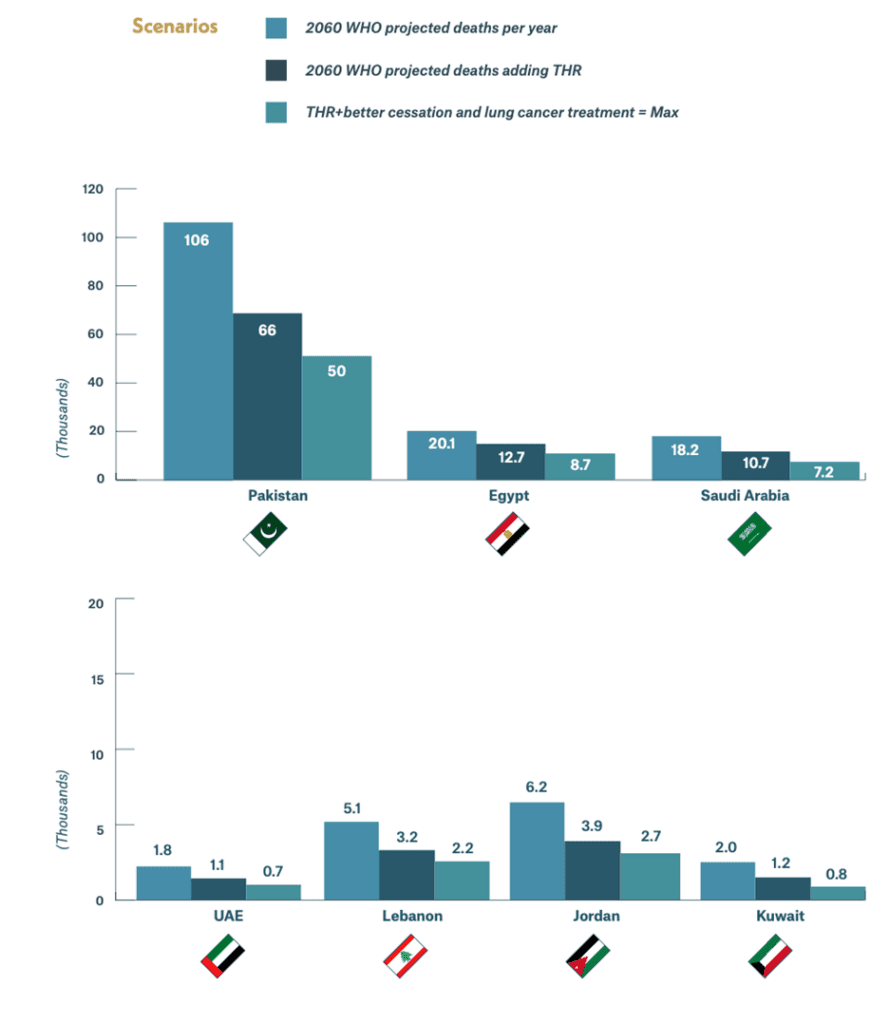
Examples of harm reduction strategies for smokers include nicotine-replacement products, such as gum or patches, and noncombustible e-cigarettes and heated-tobacco systems (HTSes). These, in addition to improving cessation rates and better access to diagnostics and treatment, have the potential to save 320,000 lives in South Africa over the next four decades.
Of course, ideally, smokers should be encouraged and assisted to quit. In fact, research shows that at least two-thirds of adult smokers want to quit or have thought about it, and almost half have actually tried in the past year. The problem is, even with assistance, quitting is very difficult—the vast majority of attempts at quitting will be unsuccessful. Furthermore, there are many smokers who just don’t want to quit. So, offering harm reduction strategies for these people makes sense. But there are oppositional voices to this.
That’s not uncommon. Despite the evident success of harm reduction strategies, there is frequently opposition to adopting them, especially where they are aimed at behaviors judged by some to be morally indefensible. Critics claimed that strategies aimed at drug “abuse” would enable “addicts,” encouraging continued drug use and causing greater harm to the community. Provision of condoms and free contraception, it was claimed, would promote sexual activity and promiscuity among young people who should be encouraged to remain abstinent until they are older.
In the same way, there are calls for access to e-cigarettes and HTSes to be restricted. It is claimed that promoting them for smoking cessation ignores the health risks associated with them and will increase vaping among children and teenagers. Vaping is seen as a gateway to combustible cigarette smoking.
There are most definitely health risks associated with e-cigarettes and HTSes. No one is denying that. Nevertheless, there is general agreement among researchers and authorities that most tobacco-related harms come from exposure to the products of combustion and that noncombustible tobacco consumption is associated with relatively fewer health risks. Furthermore, studies show that smokers who transition to e-cigarettes or HTSes are more likely to remain abstinent from combustible cigarettes.
Arguments that noncombustible products should not be available because they might be used by young people who are then more likely to become addicted to nicotine or start smoking also do not carry weight. Protecting young people from harm is obviously imperative, but that is a completely separate issue that must be dealt with in a specific manner. We cannot turn our backs on millions of adult smokers for whom a safer alternative is available that could save their lives. The message is simple: If you don’t use tobacco or nicotine-containing products, don’t start. If you do, quit. But if you can’t quit smoking or don’t want to, then switch to an alternative that carries fewer health risks. The problem is that most people, including many healthcare professionals, are unaware of alternatives to combustible cigarettes and the science showing the health benefits of switching.
If we want harm reduction to work, be it to promote healthier nutrition or physical exercise, safe sex, better hygiene and sanitation, safe housing or smoking cessation, then it has to be embedded in public health education, and people must have easy access to the elements that will make it possible. And it has to be embedded in the training of every healthcare worker so that it becomes a standard part of South African healthcare service delivery.
It’s a logical step that should seriously be considered.