A public health advocacy group based in the Philippines has criticized the latest report of the World Health Organization on the use of electronic cigarettes, saying the global body undermines the significant progress made in public health over the past two decades as smokers transitioned to smoke-free products.
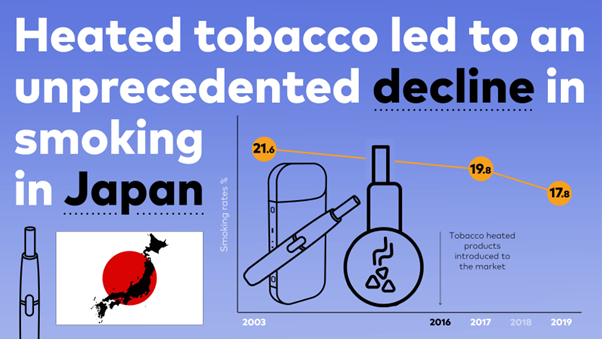
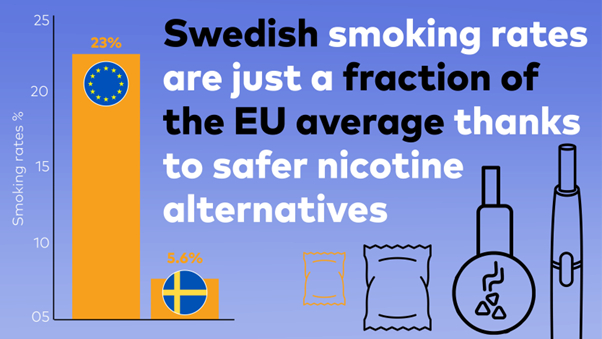
Lorenzo Mata Jr., president of Quit for Good, said the WHO’s continued demonization of e-cigarettes disregards the wealth of scientific evidence demonstrating that smoke-free alternatives such as e-cigarettes, heated tobacco and snus have helped millions of smokers in countries like the United Kingdom, the United States, Japan and Sweden successfully quit smoking.
“The best available clinical and population studies consistently show that vaping has led to adult smoking cessation. While it is necessary to monitor youth vaping, a complete ban on e-cigarettes will only exacerbate the smoking epidemic and its associated serious health conditions,” Mata Jr. said in a statement.
As a Filipino physician, Mata said the WHO’s failure to differentiate between the risks of e-cigarettes and combustible tobacco is unscientific.
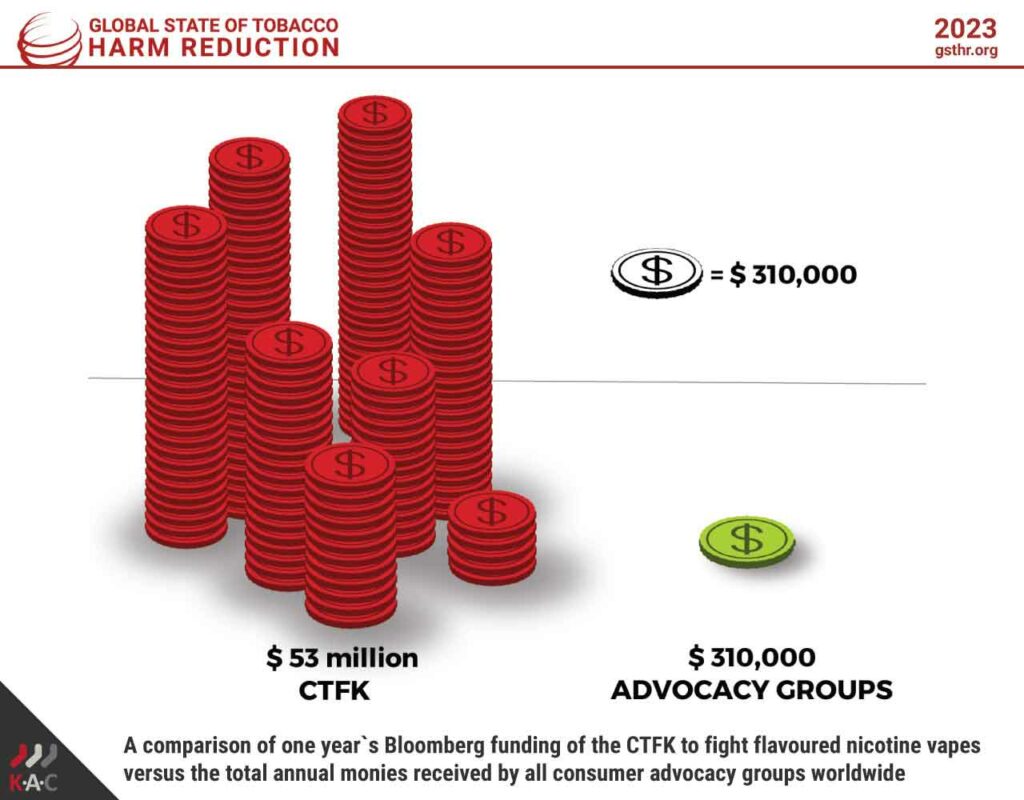
Last month, the WHO issued a statement calling for urgent action to safeguard children and prevent the adoption of e-cigarettes based on what Quit for Good insists is a misrepresented account of the scientific evidence to fit its predetermined conclusion to ban e-cigarettes or regulate them as strictly as far more dangerous cigarettes.
Additionally, the WHO provided data indicating that the global market for electronic cigarettes grew from $7.81 billion in 2015 to $22.35 million in 2022. Between 2018 and 2022, the disposable e-cigarette market expanded by 116 percent, encompassing over 550,000 different products.
Mata said the WHO’s diagnosis of the situation is flawed, as it fails to acknowledge the significant decline in harmful substance exposure resulting from smokers switching to e-cigarettes and other smoke-free alternatives, or the fact that smoke-free products work for many smokers better than traditional smoking cessation therapies.
“E-cigarettes do not threaten public health but provide smokers with an exit from smoking, which is the real problem. Labeling these innovative products an emerging threat to public health is worrisome because the WHO essentially tells smokers that continuing smoking is better than switching to e-cigarettes. This is patently wrong,” he said.
Quit for Good highlights that countries that banned e-cigarettes did not eradicate vaping but instead inadvertently created an unregulated underground market that poses risks to public health due to the absence of regulatory standards.
Mata said these bans only benefit unscrupulous criminal gangs that are happy to sell these products to anyone, including children, without any controls as to what’s in them or how they’re made.
According to independent public health experts, e-cigarettes and other smoke-free products offer an opportunity to combat smoking-related diseases such as cancer, heart disease and lung disease by transitioning to nicotine products with significantly reduced risk and no combustion.
Commenting on a similar WHO report published earlier, Peter Hajek, Director of the Tobacco Dependence Research Unit at Queen Mary University of London, said: “Given the tremendous benefits this transition would bring to public health, it is paradoxical that the WHO has adopted such a strident anti-vaping stance that risks impeding this progress. This new report perpetuates this tradition, calling for a ban on less risky alternatives while freely allowing the sale of tobacco. The report misrepresents evidence and should come with a prominent health warning.”
John Britton, an emeritus professor of Epidemiology at the University of Nottingham, said the WHO still fails to differentiate between addiction to tobacco smoking, which leads to millions of deaths annually, and addiction to nicotine, which does not.
“The WHO appears content with the inconsistency of recommending medicinal nicotine products for treating smoking addiction while advocating the prohibition of consumer nicotine products that serve the same purpose, but more effectively. The WHO is correct in discouraging non-smokers, particularly children, from using any nicotine product. However, for over a billion tobacco smokers worldwide, electronic nicotine delivery systems are part of the solution, not the problem,” Britton said.
Mata said many countries, including the Philippines, have in fact chosen to embrace scientific evidence and regulate the use of innovative smoke-free products such as e-cigarettes to provide smokers with better options to quit.


















 The Tholos Foundation, in partnership with Japan-based Pacific Alliance Institute and Sweden-based consulting firm Scantech Strategy Advisors, has released a policy paper,
The Tholos Foundation, in partnership with Japan-based Pacific Alliance Institute and Sweden-based consulting firm Scantech Strategy Advisors, has released a policy paper,