Innovation in the recreational nicotine market is disrupting not just the industry.Read More
Tags :Nicotine
A disturbingly larges share of doctors believe that nicotine causes smoking-related diseases. Read More
Critics fear the group's focus on nicotine could keep combustibles around longer.Read More
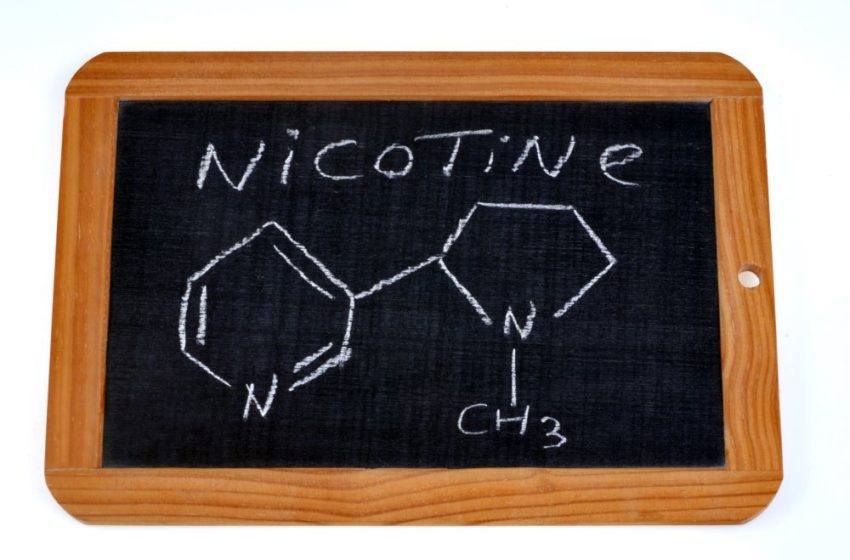
The fascinating workings of a widely misunderstood chemical. Read More
The data is being analyzed by French researchers, and the first results should be out in June.Read More
The FDA would have to release a notice and consider possible consequences, say experts.Read More
The prospects of lower nicotine levels and a ban on menthol spook investors. Read More
Japan Tobacco International insists it did not intend to target minors. Read More
Three quarters of U.S. adults incorrectly believe nicotine causes cancer, says Altria. Read More
The proposed rule was removed from the agenda late last year without significant explanation. Read More